A Developer's Guide to Clinical Informatics
Clinical informatics is where information science, computer science, and healthcare collide. It’s the practical art and science of taking raw, messy health data and transforming it into something useful—something that can actually improve a patient's care, make a hospital run more smoothly, or even fast-track medical research.
For those of us on the development side, this field isn't just an abstract concept. It's a massive opportunity to apply our skills to problems that have a real human impact.
A Blueprint for Modern Healthcare

Imagine a modern healthcare system as a complex, sprawling smart city. A city can't function without its underlying infrastructure—the roads, power grids, and communication lines that connect everything. In this world, clinical informatics is the intelligent infrastructure that makes the entire healthcare system work.
Without it, you just have a collection of isolated buildings. Think of hospitals, clinics, and labs as disconnected islands, each holding pieces of a patient's story—lab results here, prescriptions there, a doctor's notes somewhere else. This fragmentation creates data silos, making it nearly impossible to see the complete picture.
Clinical informatics is what builds the bridges and highways between these silos. It creates the common language and the rules of the road that allow information to move securely and logically from point A to point B. This structured data flow is the magic that lets a doctor instantly see a patient's full history or allows a researcher to analyze population-level data to discover a new treatment. This is exactly where your skills as a developer or data engineer become critical.
The Developer's Role in Building the System
Your technical expertise is what brings this digital city to life. Developers and data engineers are the crews designing the data pipelines, building the analytical tools, and making sure the whole system is robust and secure.
This isn't a niche field anymore. The clinical informatics market is projected to skyrocket to USD 485.32 billion by 2030. This growth is fueled by a desperate need for professionals who can manage enormous volumes of health data. The demand is particularly intense in North America, which currently accounts for a dominant 49.9% market share.
This guide is designed to be your roadmap. We’ll break down:
- Core Concepts: Get a handle on the terminologies, standards, and data models that are the bedrock of health data.
- Real-World Workflows: See how data moves from raw EHR exports to sophisticated AI-driven predictive models.
- Modern Tooling: Learn how platforms can radically speed up your work, with practical advice and examples.
- Career Pathways: Discover the key roles and skills that will help you build a career in health tech.
By the time we're done, you'll have a clear, practical understanding of how your code directly contributes to building a smarter, more connected healthcare ecosystem. Mastering these concepts is a crucial first step toward delivering better healthcare interoperability solutions.
Decoding the Language of Healthcare Data
To get your bearings in clinical informatics, you have to start with the fundamental building blocks of health data. It's a bit like learning a new language. You can't write complex sentences until you know the vocabulary, grammar, and structure. In healthcare, these core components are terminologies, standards, and data models.
These three pillars are what turn messy, inconsistent information into a structured, reliable asset. Getting a handle on them isn't just academic; it's essential for anyone building applications, running analytics, or managing data pipelines in this field. Without this foundation, you’re just guessing.
Terminologies: The Universal Dictionaries
At its core, a clinical terminology is just a standardized vocabulary. It assigns a single, clear meaning to a clinical idea, making sure a diagnosis recorded in Tokyo means the exact same thing as one in Toronto.
Terminologies are the bedrock of interoperability. They ensure that when one system says 'myocardial infarction,' another system doesn't interpret it as just 'chest pain.' This precision is critical for patient safety and large-scale research.
For instance, doctors might describe the same condition using different phrases like "Type 2 diabetes," "T2DM," or "adult-onset diabetes." A terminology like SNOMED CT solves this by mapping all those variations to a single, unique code, eliminating any guesswork.
To help clarify, here’s a quick rundown of the most common terminologies you'll run into.
Key Terminologies in Clinical Informatics
| Terminology | Primary Domain | Example Use Case |
|---|---|---|
| SNOMED CT | Clinical Findings, Procedures, Diseases | Describing a patient's diagnosis of "acute bronchitis" with a universal code. |
| LOINC | Laboratory Tests & Clinical Observations | Uniquely identifying a "Hemoglobin A1c" lab test result across different systems. |
| RxNorm | Medications | Connecting the brand name drug "Tylenol" to its ingredient "acetaminophen." |
| ICD-10-CM/PCS | Diagnostics & Procedures (Billing) | Coding a patient encounter for insurance reimbursement for "strep throat." |
| CPT | Medical Procedures & Services (Billing) | Specifying a "standard office visit" for billing purposes. |
Each vocabulary serves a specific purpose, and knowing which one to use is half the battle. This is especially true when tackling challenges like EHR Integration, where a clear understanding of data's meaning is non-negotiable.
Standards and Models: The Rules of Engagement
If terminologies are the words, then standards and data models are the grammar and sentence structure. Standards provide the rules for exchanging information, while data models create a consistent structure for storing it.
Think of data exchange standards like HL7 and its more modern counterpart, FHIR (Fast Healthcare Interoperability Resources), as secure couriers for health data. They define the message formats and APIs that let different software systems talk to each other without losing information in translation.
A Common Data Model (CDM), on the other hand, provides a standardized database layout. This means that no matter where the data came from—an EHR, a claims database, a patient registry—it gets organized in the exact same way. The OMOP Common Data Model is a prime example, built to transform disparate datasets into a uniform format that's ready for analysis right out of the box.
This diagram from OHDSI shows it perfectly: a CDM funnels messy, varied source data into a single, clean structure.
This model is a powerful translator, making large-scale, reproducible research possible by ensuring everyone is analyzing data that's structured identically.
Practical Tips for Working with Vocabularies
Getting comfortable with these concepts is one thing; using them effectively is another. Here are a few tips to get you started on the right foot:
- Focus on the Use Case: Don't get bogged down memorizing codes. Instead, know which tool to grab for the job. Use RxNorm for medication data, LOINC for labs, and SNOMED CT for building clinical cohorts.
- Explore Vocabulary Browsers: Get your hands dirty with online tools that let you explore these terminologies. Seeing how concepts are linked and organized is key to understanding how to map data correctly.
- Automate Your Mapping: Mapping data manually is a recipe for slow, error-prone work. It's worth learning about automated techniques; you can find a good primer on this at https://omophub.com/blog/semantic-mapping.
- Use Managed Vocabulary Services: These vocabularies are enormous and constantly updated. Trying to maintain them yourself is a huge technical headache. An API-first platform like OMOPHub handles all that for you, letting you focus on the data, not the infrastructure. For advanced queries, like finding relationships between concepts, check the OMOPHub API documentation.
Mapping a Real-World Clinical Informatics Workflow
Knowing the building blocks of clinical informatics—terminologies, standards, and data models—is like having the blueprints. Now, let’s see how they all come together in a real-world workflow, following data from a patient’s bedside all the way to a research-grade database. The journey is rarely a straight line; it's often messy and full of the kind of roadblocks every developer in this space learns to anticipate.
Everything starts with raw data, which is usually locked up in different systems. The main source is almost always the Electronic Health Record (EHR), the digital story of a patient's care. In fact, EHRs are so central to the field that they command a 36.4% market share in 2024. This growth is fueled by global pushes for digital records and the need for systems to talk to each other, making the EHR the heart of most health IT projects. You can find more market analysis from firms like SNS Insider.
The First Hurdle: Extract, Transform, Load (ETL)
The first real step in any clinical data project is getting your hands on the data through a process known as Extract, Transform, Load (ETL). This is where you get your first taste of just how messy healthcare data can be.
- Extract: You start by pulling data from its source, whether that's an EHR, a lab information system (LIS), or a billing database. The catch? Each system has its own weird format, structure, and set of local codes.
- Transform: This is the make-or-break stage. Here, the raw, inconsistent data has to be cleaned up, validated, and—most importantly—mapped to a standard format and vocabulary.
- Load: Once the data is clean and standardized, it’s loaded into its final destination, usually a database built on a common data model like OMOP.
This process is all about turning chaotic, disconnected data points into a single, coherent dataset that’s ready for analysis. The diagram below shows how the foundational pillars of informatics guide this transformation.
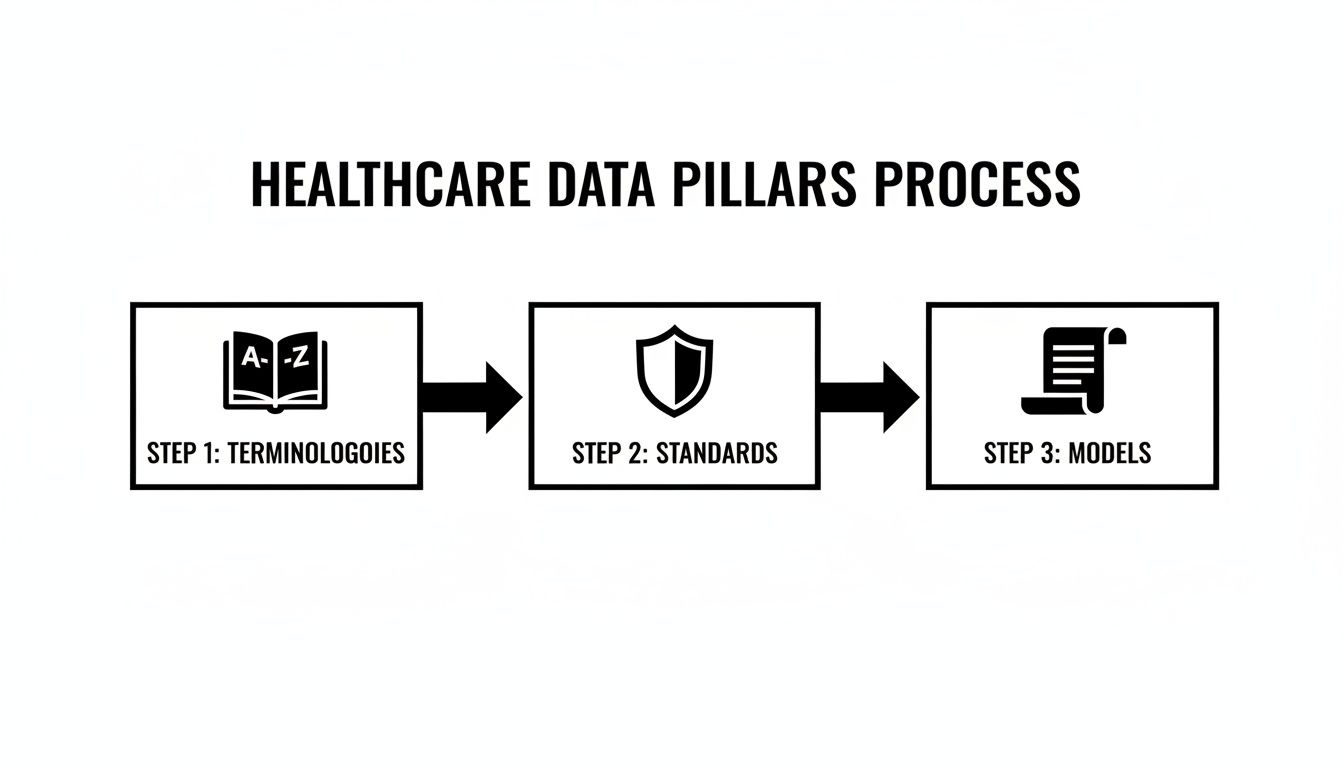
As you can see, terminologies give us the language, standards provide the rules, and models supply the structure—everything you need to bring order to the chaos.
The Art and Science of Vocabulary Mapping
The real magic happens in the "Transform" stage, specifically during vocabulary mapping. This is where you translate all those proprietary, local codes into globally understood standard terminologies.
For instance, a hospital might use its own internal code "HC-123" for a diagnosis of "Headache, chronic." For that data to mean anything to someone outside that hospital, you have to map "HC-123" to its official SNOMED CT concept ID, which is 73430006.
Without accurate vocabulary mapping, data stays stuck in its silo, ambiguous and unusable for larger-scale research. It’s the critical step that allows researchers to combine data from different hospitals and be confident that "headache" means the same thing everywhere.
This is a tough, meticulous process. A single dataset can have tens of thousands of local codes for drugs, procedures, and conditions. Mapping them all by hand is simply out of the question, which is why programmatic tools and a deep familiarity with the terminologies are absolutely essential.
From Standardized Data to Actionable Insights
Once the data is cleaned, mapped, and loaded into a common data model, you can finally unlock its true potential. This newly structured information becomes the fuel for all kinds of applications that are at the core of clinical informatics.
-
Analytics and Reporting: Analysts can now query the unified dataset to build dashboards for hospital administrators, track quality metrics, or monitor patient outcomes. For example, they could easily analyze post-surgery infection rates across different departments.
-
Clinical Research: Researchers can find specific patient groups for clinical trials with incredible speed. A query that used to involve months of manually reviewing charts—like finding all male patients over 50 with Type 2 diabetes on a specific medication—can now be done in minutes.
-
Predictive AI and NLP: High-quality, standardized data is the perfect training ground for machine learning. Teams can build predictive models to forecast disease outbreaks, identify patients at high risk for readmission, or use Natural Language Processing (NLP) to pull meaningful information out of unstructured clinical notes.
Each stage in this workflow is built on the one before it, ultimately turning raw clinical entries into a powerful asset that can drive better care and speed up medical discovery.
Tips for a Smoother Workflow
Getting through this process is never without its challenges. Here are a few practical tips to help you sidestep common pitfalls and build more effective data pipelines.
- Understand Your Source Data First: Before you write a single line of ETL code, sit down with the clinicians and analysts who use the source system. Learn its quirks, its limitations, and what each field actually means in practice.
- Use an API-First Vocabulary Service: Don’t try to maintain local copies of massive vocabularies like SNOMED CT. It’s a huge infrastructure headache. A service like OMOPHub gives you instant API access, which you can see in the OMOPHub API documentation.
- Automate Mappings with SDKs: Take advantage of tools like the OMOPHub Python SDK or the OMOPHub R SDK to programmatically search for and map concepts. This cuts down on manual work and drastically improves accuracy.
- Iterate and Validate Constantly: Your ETL and mapping logic won't be perfect the first time around. Build a continuous feedback loop with subject matter experts to catch errors early and refine your process over time.
How Modern Tools Are Fixing a Broken Workflow
Anyone who has worked in clinical informatics knows the old way of managing vocabularies is a huge bottleneck. The traditional approach—downloading, hosting, and trying to maintain massive local databases—is a grind. It’s slow, sucks up resources, and is a nightmare for version control. This model forces data teams to spend more time playing sysadmin than actually generating insights, dragging down the entire workflow from ETL to analysis.
Thankfully, that's changing. Modern, API-first platforms flip this dynamic on its head. Instead of wrestling with a clunky local setup, developers can now access up-to-date terminologies programmatically. This isn't just an incremental improvement; it's a fundamental shift in how we build and manage clinical data pipelines.
The Inevitable Shift to the Cloud
This move toward more nimble tooling is happening across the board. Cloud-based deployments are quickly becoming the standard in clinical informatics, and for good reason. They are set to grow at the fastest rate through 2030 and are projected to hold a 45% share in the health informatics market by 2025.
This is a massive industry, expected to hit USD 683.11 billion by 2032, and cloud solutions are a huge part of that growth. EHR integrators and AI/ML teams love the flexibility, scalability, and cost-effectiveness. The cloud just makes sense—it gets rid of the local hosting headache while providing seamless updates and robust security. For a deeper look at these market dynamics, you can explore the full health informatics market report.
Platforms like OMOPHub are built precisely for this reality. They offer global edge performance with sub-50ms response times without a single thing to install locally. This frees up teams to focus on what actually matters: mapping data, building analytics, and developing models.
From Manual Drudgery to Programmatic Precision
Let's walk through a common, real-world task: mapping a local lab code to its standard LOINC equivalent. In a traditional setup, this was a manual chore. You'd have to search a local database or a clunky web browser, a process that’s both tedious and completely unscalable.
With a modern toolset, this becomes a simple, automated step in your ETL script. A dedicated SDK lets you handle the mapping with just a few lines of code.
Here’s a hands-on example using the OMOPHub Python SDK. Let's say you have a local lab test named "HGB A1C" and need to find its standard LOINC code.
from omophub.client import Client
# Initialize the client with your API key
client = Client(api_key="YOUR_API_KEY")
# Search for the concept in the LOINC vocabulary
try:
results = client.concepts.search(
query="HGB A1C",
vocabulary_id=["LOINC"],
concept_class_id=["Lab Test"]
)
# Print the top result's concept details
if results.items:
top_result = results.items[0]
print(f"Concept Name: {top_result.concept_name}")
print(f"Concept ID: {top_result.concept_id}")
print(f"Vocabulary: {top_result.vocabulary_id}")
else:
print("No results found.")
except Exception as e:
print(f"An error occurred: {e}")
This code snippet automates what was once a manual, error-prone task. By integrating vocabulary lookups directly into data pipelines, teams can process millions of records with speed and consistency, ensuring data quality from the very beginning.
This simple script connects to the OMOPHub API, searches LOINC for "HGB A1C," and pulls back the standard concept. The whole thing is handled programmatically. You can embed this logic directly into your ETL workflows and map thousands of codes automatically. For anyone working with AI in healthcare, this kind of automation isn't just a nice-to-have; it's the foundation for building any kind of advanced model.
Practical Tips for Sharpening Your Workflow
Integrating modern tools can give your team a serious efficiency boost. Here are a few practical tips to get started:
-
Use SDKs to Automate Everything: Don't make raw API calls if you don't have to. Official SDKs for Python or R handle the messy parts like authentication, error handling, and data parsing, which really cleans up your code. You can find the official SDKs on GitHub for Python and R.
-
Dig into the Documentation for Power Features: Go beyond simple searches. Modern vocabulary services have powerful features for exploring concept relationships, finding ancestors, or performing cross-vocabulary mappings. The OMOPHub documentation is full of detailed examples for these advanced use cases.
-
Map Your Vocabularies Early and Often: Do your terminology mapping as early as you possibly can in your data pipeline. This step ensures that every downstream process—from loading data into an OMOP CDM to building analytical models—is working with clean, standardized data from the get-go. If you're new to this framework, you can learn more about the OMOP Common Data Model in our article to get a handle on its structure.
Building Your Career in Clinical Informatics
So, you're a developer or data pro looking to work on problems that genuinely matter. Clinical informatics isn't just another tech niche; it's a field where your code and analytical skills can directly impact patient care. But breaking in means figuring out where your specific talents fit best.
Let's walk through the core roles you'll find on most clinical informatics teams. While the job titles might differ from one hospital or research institute to another, the fundamental responsibilities usually fall into a few distinct buckets. Each role is a crucial piece of the puzzle, working together to turn messy clinical data into something that can actually improve health outcomes.
The Clinical Data Engineer: Architect of the Data Flow
The Clinical Data Engineer is the one in the trenches, building the infrastructure that makes everything else possible. Their job is to architect the data pipelines that pull raw information from various sources—think electronic health records (EHRs), lab systems, and billing platforms—and funnel it into a clean, usable analytical environment.
Day-to-day, this means writing a lot of SQL and Python. They spend their time building robust ETL (Extract, Transform, Load) processes, wrangling gnarly, inconsistent data, and ensuring that what lands in the common data model is something the team can actually trust. A data engineer's success is measured by the reliability and scalability of the systems they build.
The Clinical Analyst: Storyteller and Insight Generator
If the engineer lays the pipes, the Clinical Analyst is the one who finds the valuable insights in the water flowing through them. This role is all about answering critical questions for clinicians, researchers, and hospital leadership by digging into the standardized data.
Their main tools are SQL for querying, visualization platforms like Tableau for building dashboards, and statistical software for deeper analysis. One day they might be creating a dashboard to monitor hospital readmission rates; the next, they could be identifying a specific cohort of patients for a new clinical trial. They are the translators, turning complex clinical questions into data queries and presenting the answers in a clear, actionable way.
An analyst's main job is to bridge the gap between the data and the decision-makers. They find the story hidden within the numbers and use it to drive improvements in patient care or operational efficiency.
The Informatics Specialist: The Translator and Bridge
The Informatics Specialist (or Informaticist) is the vital link connecting the technical team with the frontline clinical staff. Many specialists come from a clinical background themselves—nurses, pharmacists, or physicians who have cross-trained in IT. This dual perspective is their superpower.
They understand the realities of clinical workflows and can translate a doctor's needs into a concrete set of requirements for the engineers and analysts. They're heavily involved in workflow analysis, implementing new systems, and training end-users, ensuring that the technology being built actually solves a real-world problem and doesn't just create more clicks for a busy nurse.
Tips for Finding Your Path
Ready to find your place? Here are a few practical steps to get started.
- Play to Your Strengths: Are you passionate about building resilient, high-performance systems? The data engineering track is likely for you. Do you love the thrill of the hunt, asking tough questions and uncovering hidden patterns? An analyst role would be a great fit.
- Learn the Language of Healthcare: You don't need to go to med school, but you absolutely have to get comfortable with clinical terminologies. It's the lingua franca of the field. Resources like the OMOPHub documentation are a great place to start learning your way around vocabularies like SNOMED CT and LOINC.
- Build a Portfolio Project: Nothing speaks louder than demonstrated skill. Grab a public healthcare dataset and get your hands dirty. Use tools like the OMOPHub Python SDK or the R SDK to perform some vocabulary mapping and build a simple dashboard. This is a powerful way to show a potential employer that you can do the work.
Navigating Security and Compliance in Healthcare

In clinical informatics, data security isn't just a technical detail—it's the very foundation of patient trust. We're dealing with Protected Health Information (PHI), and the rules governing it are ironclad. A single mistake can shatter that trust and lead to crippling consequences, with fines easily running into the millions.
As a developer, this isn't someone else's problem to solve. Understanding these regulations is a fundamental part of building any responsible and viable healthcare technology.
Two regulatory giants shape the field: the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) across Europe. While they have their differences, their core mission is the same: protect patient privacy by setting strict rules for how data is handled. These aren't guidelines; they're legal mandates for any system that touches patient data.
Core Security Practices You Must Implement
Meeting these demands requires a few non-negotiable security practices. Think of these as the technical bedrock for any secure clinical informatics system, turning compliance from a dreaded checklist into a functional part of your architecture.
Here's what that looks like in practice:
- End-to-End Encryption: Data has to be unreadable both when it's moving across a network (in transit) and when it's sitting in a database (at rest). If someone manages to intercept it, it should be nothing but gibberish.
- Role-Based Access Control (RBAC): This is just the principle of least privilege. People should only be able to see and do what is absolutely necessary for their job. A billing clerk, for instance, has no business accessing a patient's detailed clinical notes.
- Immutable Audit Trails: Every single action taken on sensitive data—every view, every query, every change—must be logged in a way that can't be tampered with. These logs are your system's black box, absolutely essential for any security investigation or compliance audit.
Platforms with built-in compliance features are a developer’s best friend. They handle the complex, undifferentiated heavy lifting of security, allowing you to focus on building features instead of worrying about regulatory pitfalls.
How Your Tools Can Simplify Compliance
The right technology stack can dramatically lighten the compliance load. A platform that was built from the ground up with healthcare security in mind will have these safeguards baked in, not just bolted on as an afterthought.
Take a service like OMOPHub, for example. It provides immutable audit trails with a seven-year retention period right out of the box. This single feature helps organizations meet HIPAA’s demanding record-keeping requirements automatically, without any extra development effort.
This built-in approach doesn't just make development easier; it significantly reduces organizational risk. When your vocabulary service already enforces encryption and logs every API call, your team can build with the confidence that they're on solid ground.
Tips for Maintaining a Secure Environment
- Understand Data De-Identification: Get familiar with the difference between anonymized and pseudonymized data. For analytics and research, true anonymization—where every possible identifier is stripped away—is often the safest route.
- Review Vendor Compliance: If you bring a third-party service into your stack, you must verify their compliance. Look for a signed Business Associate Agreement (BAA) for HIPAA or a Data Processing Addendum (DPA) for GDPR.
- Regularly Audit Access Logs: Don't just collect audit trails and let them gather digital dust—actually review them. You can dive deeper into these practices in the official OMOPHub security documentation. Using SDKs like the OMOPHub Python SDK or R SDK helps ensure every interaction is logged securely and consistently.
Answering Your Top Questions About Clinical Informatics
As more developers and data scientists dip their toes into health tech, a few questions always seem to pop up. It's a field with its own language and rules, so getting your bearings early on can save you a lot of headaches. Let’s tackle some of the most common ones head-on.
What's the Real Difference Between Bioinformatics and Clinical Informatics?
It's easy to get these two confused since they both sit at the intersection of biology, data, and computers. The simplest way to think about it is this: bioinformatics is about the molecules, while clinical informatics is about the patient.
Bioinformatics dives deep into the raw biological code of life—genomics, proteomics, and all the other "-omics." Researchers in this space are often trying to answer fundamental scientific questions. On the other hand, clinical informatics takes the data generated during actual patient care (think EHRs, lab results, doctor's notes) and uses it to make healthcare better, safer, and more efficient. One is discovery-focused; the other is application-focused.
Which Programming Languages Actually Get Used?
If you want to be effective in this field, you need a solid technical toolkit. While you can find a use for almost any language, three are the undisputed workhorses of clinical informatics.
- SQL: This is your bread and butter. Seriously, it's non-negotiable. So much of your time is spent pulling, cleaning, and organizing data from relational databases, and SQL is the language for that job.
- Python: The jack-of-all-trades for data work. With libraries like Pandas for data wrangling and Scikit-learn for machine learning, Python is what you'll use to build complex data pipelines and predictive models.
- R: A favorite in academic and research circles for a reason. R is a powerhouse for hardcore statistical analysis, data visualization, and the kind of epidemiological studies that are common in healthcare research.
Get comfortable with these three, and you'll be well-equipped to handle just about any technical challenge that comes your way.
How Do I Get Started with the OMOP Common Data Model?
Jumping into a massive framework like OMOP can feel overwhelming. The trick is to not try and boil the ocean. Start with a manageable piece and build from there.
Expert Tip: Don't start with the data model itself—start with the vocabularies. Getting a feel for how terminologies like SNOMED CT and LOINC are organized is a much better entry point than wrestling with a full-scale ETL process right away.
Here’s a practical way to begin:
- Play with the Vocabularies: The best way to learn is by doing. Use an API-first platform to search for concepts and see how they connect to each other. You can find some great starter examples in the OMOPHub API documentation.
- Try a Mini-Mapping Project: Grab an SDK in a language you already know, like the OMOPHub Python SDK or the OMOPHub R SDK. Write a small script that takes a handful of your local codes and maps them to standard OMOP concepts. This simple exercise builds the core skills you'll need for much larger projects down the road.
Ready to stop wrestling with vocabulary databases and start building faster? With OMOPHub, you get instant, programmatic access to standardized terminologies through a simple API, eliminating the infrastructure burden. Get your API key and start building in minutes at https://omophub.com.